Got PCOS? Get these important labs
If you have PCOS, you’ve probably been through the ringer (that’s washing machine for you young folks) to get diagnosed.
Your doctor might have even diagnosed you on symptoms alone - not a great idea, since PCOS and several other conditions have similar symptoms. You deserve answers, and answers come by getting labs. Since I find myself giving people this list all the time, it’s time to write a blog post and share it with the world!
Things to know about PCOS labs
If your doctor is thorough, they will do an ultrasound to check for “cysts” (they aren’t really cysts, but that’s another blog post) to confirm your diagnosis - unless you don’t have any. Which, it’s totally possible that you don’t have cysts AND you still have PCOS. Since PCOS is a syndrome, its inclusion criteria have been debated. It’s generally agreed that you have to have 2 of these 3 things to get a diagnosis:
Ovarian “cysts”
High testosterone and/or androgens
Irregular periods
Here’s the thing though - knowing which symptoms you have doesn’t mean you know how to treat them!
If you’re like most people with PCOS, your doctor said “Here’s a prescription for birth control, come back and see me when you want to have kids.”
…Except you might not want to take hormones to regulate your cycle for a variety of reasons. Or, you might not want to have kids. So what’s an intellectual progressive supposed to do?
Educate yourself. I know, it sucks that the burden falls on you. This is how it usually goes with chronic illnesses (especially for people with uteri). You have to be your own advocate. And if you’re lucky, you can partner with a doctor who understands PCOS and is dedicated to helping you feel your best regardless of the methods you prefer to get there.
So in the name of knowledge, here’s a list of labs to request.
Keep in mind that a PCP (regular doc) might look at you funny when you ask for some of these - they may not know why they are relevant. It’s really helpful to work with a gynecologist or endocrinologist who specializes in PCOS for this reason - less pushback. But ultimately, you are the boss and can get whatever labs you ask for, if you’re willing to pay for them.
With a PCOS diagnosis, insurance should cover most of these, and if your doc is extremely unhelpful, you can potentially get your labs done at a walk-in lab (Any Lab Test Now!) or at home via a blood-spot test (EverlyWell).
What to test if you have PCOS
Complete Blood Count (CBC)
This is standard when you go in for a physical. If you haven’t had this done in awhile, it’s important - these immune markers can be altered if you are fighting off a mild infection. In functional medicine/nutrition, we assess the CBC first because it can tell us a lot about what to expect from more specific lab work.
Comprehensive Metabolic Panel (CMP)
On the surface, this series shows your electrolyte status as well as kidney and liver function. But you may be able to get more info, like if your adrenals are working harder than usual to keep everything going, if your body is dumping calcium due to chronic stress/estrogen issues, or if your sodium is a little off because of overexercising.
Complete Thyroid Panel
This series might be harder to get - and potentially only necessary if you have symptoms of thyroid issues. But it’s really common in PCOS to have hypothyroid as an underlying cause or cofactor, and it often goes undiagnosed. That’s why you want to get the full panel (TSH, free T3, free T4, reverse T3, and antibodies) done - you may have subclinical hypothyroid that TSH alone won’t be able to assess. Treatment for hypothyroid can make a big difference in how you feel!
Lipid Panel
Unfortunately, PCOS comes with increased risk for other diseases, including cardiovascular disease. This is likely because people with PCOS often have a MTHFR gene mutation that increases likelihood of oxidative stress, DNA replication issues, and cardiovascular inflammation. These gene makes it harder for you to take folic acid and turn it into folate - the active form of the vitamin. Since folate is critical for hundreds of functions in your body, the effects of MTHFR variations are extensive. A lipid panel can help you get ahead of any complications, such as elevated LDL cholesterol, or HDL cholesterol that is too low to be protective. Triglycerides are also relevant here, since elevated blood glucose or insulin resistance is a strong predictor of elevated triglycerides. I recommend also requesting VLDL - knowing your cholesterol particle size can be very helpful when deciding how aggressive to be with nutrition and lifestyle changes.
Inflammation status
C-reactive protein (CRP) - if you have elevated cholesterol, this marker may also be high. It can tell you how much inflammation your body is producing in response to the stress it’s under, and can help you decide the most important actions to take for your health.
Homocysteine - another inflammation marker that’s related to MTHFR status.
Hormone Panel
If you have PCOS, you have altered reproductive hormones. The “fun” part is figuring out which hormones are too high/low. What’s “normal” varies widely because bodies are unique, but in general there are some important things to assess.
Estrogen - too high can contribute to the lovely PMS experience, too low can make it impossible to ovulate or feel juicy.
Progesterone - it’s common for this hormone that regulates your period to be too low in PCOS.
Testosterone - yours might be high, or it might not! Make sure you test free T (the amount of testosterone that’s actually usable by your body), not just total T.
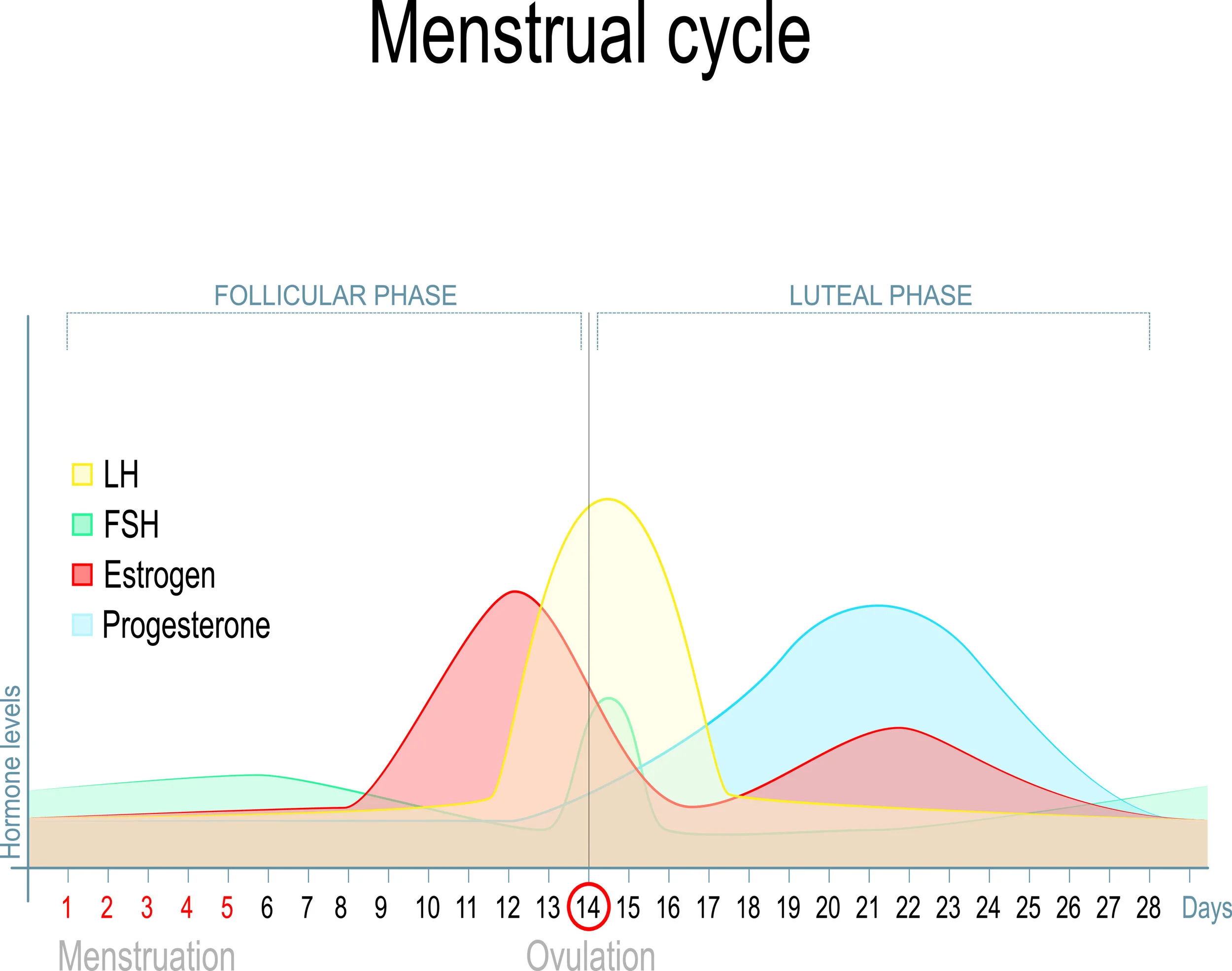
Luteinizing hormone (LH) - it’s supposed to be low early in your cycle and surge right before ovulation, but any changes in that will keep you from ovulating and affect egg quality (if that’s important to you).
Follicle Stimulating Hormone (FSH) - tells your body to mature eggs before you ovulate, and if it’s too high or low, ovulation can be delayed or cancelled. Even if you don’t want to get pregnant, this matters because it affects your hormonal health and your cycle.
DHEA - this hormone precursor is an androgen that might be high even if your testosterone is normal, and that can explain some of your symptoms as well as the root cause behind your PCOS.
SHBG - this protein binds to your hormones to transport them around your body, but if levels are high you may have a whole lot of inactive hormones in your body (making them useless).
Hormones fluctuate throughout your cycle, so when you test matters. Try to get a baseline test done on day 3 after your period starts. If you suspect you have estrogen dominance or have difficulty conceiving after ovulation, a test 7 days after ovulation is useful as well. If you don’t have regular periods or are on birth control, it’s ok to test whenever.
Glucose regulation
HbA1c - This test is a general average of how high your blood sugar has been over the past 3 months. It’s a much better assessment of your glucose regulation than fasting glucose!
Fasting insulin or insulin tolerance test - If you have normal fasting glucose and an average or slightly high HbA1c, but have symptoms of glucose dysregulation (afternoon fatigue, skin tags, velvety skin patches), you may have insulin resistance that isn’t showing up strong enough in the glucose tests. Check out your fasting insulin, or have an insulin tolerance test, in order to assess how aggressively you want to treat your glucose regulation.
Nutrient status:
Vitamin D - this potent hormone-like substance supports normal blood sugar, immune system, thyroid, and reproductive hormone status. Most docs will say you’re “fine” even if your number is lower than optimal. I recommend 50+ to support healthy hormones!
Vitamin B12 - if you have MTHFR, chronic fatigue, or a super active lifestyle, you may be insufficient in B vitamins. While testing them all would be amazing, most docs only offer B12 and it can give you a good idea of where you might be with other B vitamins.
Whew! That’s a lot - and there’s even more you could do! But these are the tests I recommend most often to my clients with PCOS.
Once you’ve got your tests done, it’s important to interpret them properly. Ask your doctor to walk you through each result, or work with a qualified functional medicine nutritionist/dietitian to help you decide what to do with the results. It can get overwhelming, so take a deep breath and start with the most important stuff, then work your way out from there.
Looking for guide to help you along your PCOS journey?
Nutrition Therapy does exactly that. It’s a deep dive into all the things that affect your hormones and practical steps you can take to optimize your situation - even if you’re struggling with severe symptoms!
You’ll get 3-6 months of lab assessment, movement coaching, lifestyle guidance, supplement implementation, and body image rehab - perfect for people with PCOS.
In fact, while I work with folks with a variety of health concerns, most of my clients have PCOS! They’ve been able to get rid of afternoon fatigue, improve their relationship with movement, build body confidence, ditch the scale, and start nourishing their body in a loving supportive way.
It’s as amazing as it sounds! Click here to learn more, and sign up for a free chat with me so we can decide together if nutrition therapy is right for you.
Much love and hugs,